In Clinical
Let’s get clinical. Follow the links below to find out more about the latest clinical insight in community pharmacy.Bookmark
The global Sore Throat and Antibiotic Resistance (STAR) study, which included participants from the UK, surveyed 12,000 people aged 18-64 years who had treated respiratory symptoms in the preceding six months. Fifty-three per cent of these had taken antibiotics.
“In Europe, great efforts are being made to address the antimicrobial resistance [AMR] problem. For example, data from the latest Eurobarometer show that antibiotic use in the EU is decreasing, but much remains to be done,” says Dr Elsa López-Pintor from the Faculty of Pharmacy, University Miguel Hernández de Elche, Alicante, Spain.
“In particular, there is significant room for improvement in the management of sore throats, which is probably the minor symptom where there is the greatest overuse of antibiotics.”
Pharmacists and AMS
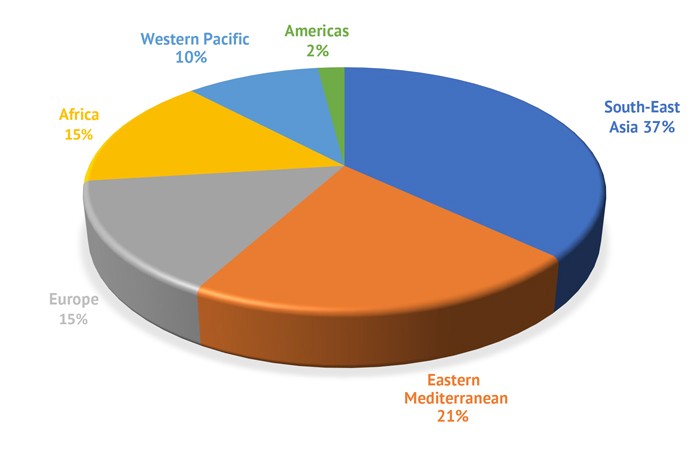
Dr López-Pintor was an author of a study presented in September at the International Pharmaceutical Federation annual congress in Seville, Spain. The study, sponsored by Reckitt, surveyed 794 pharmacists (Figure 1). Globally, 85 per cent of pharmacists said they want a greater role in anti- microbial stewardship (AMS) for URTIs.
“There are many differences between countries: we must learn from the experiences of those that have taken action and are leading the way,” says Dr López-Pintor, who is a member of GRIP, an expert-led initiative founded by Reckitt.
“Initiatives by pharmacists in Europe focus on ensuring responsible, safe and evidence-based use of antimicrobials in the community by leveraging communication channels, such as the internet and social media, developing strategies to rationalise antimicrobial consumption and minimise AMR, and supporting the advancement of the pharmacist workforce.
“In turn, some UK initiatives are good examples for other partners, such as the Pharmacy Quality Scheme’s antibiotic prescribing checklist for community pharmacy [England], the Pharmacy First minor ailments service [Scotland] and the Keep Antibiotics Working campaign.”
Ninety-six per cent of pharmacists indicated that they would be interested in attending educational courses about optimising antimicrobial use.
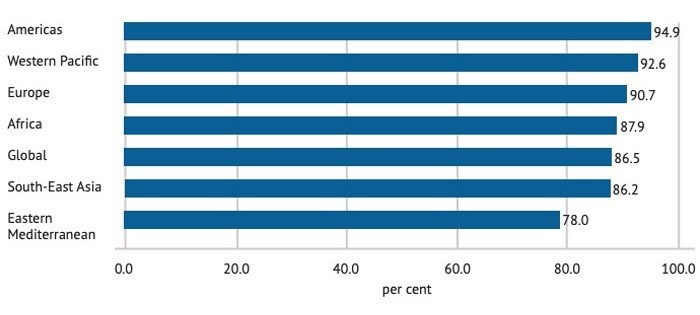
The survey also found that 87 per cent of pharmacists globally believed that patient education about appropriate antimicrobial use and the need for AMS were important. Rates differed between regions (See Figure 2 below).
“The worrying lack of public awareness of the appropriate use of antibiotics is perhaps one of the biggest problems,” says Dr López-Pintor. “Strategies that highlight and reinforce pharmacists’ role as educators, helping to raise awareness of the problem of AMR and the need to preserve antibiotics for situations where they are really needed, are necessary.”
PoC testing
The survey found that 58 per cent of pharmacists were willing to use point-of-care throat-swab testing for Streptococcus A, which caused the recent outbreak of scarlet fever (see also p32), to inform treatment in patients with sore throats – but only 12 per cent can access these tests.
Commenting on the results, Dr Martin Duerden from the University of Cardiff and adviser to the Royal College of GPs and NICE pointed out that some UK pharmacies can provide point-of-care testing for streptococcal infection in sore throats through various initiatives and enhanced services. “There has also been interest in use of point-of-care C-reactive protein testing for respiratory tract infections through pharmacy enhanced services.”
“In the absence of point-of-care testing, the FeverPAIN or Centor criteria [see below] can help identify those who are most likely to benefit from an antibiotic when the sore throat is caused by a streptococcal bacterial infection,” says Dr López-Pintor, “and those who should be referred to a GP.”
Both Dr López-Pintor and Dr Duerden agree that community pharmacists are central to AMS for URTI. “Pharmacists should ask about symptoms to help people decide whether they would benefit from antibiotics and/or advise them on other ways to relieve symptoms, such as taking painkillers, medicated lozenges and drinking fluids,” Dr López-Pintor suggests.
“We know that rapid and effective symptomatic relief is important to meet patients’ expectations and avoid unnecessary antibiotic use – so pharmacists should manage evidence-based consensus protocols that aid decision-making in acute sore throat, such as NICE guidance.”
Best practice
“Learning resources and patient-friendly materials to aid conversations with patients can support AMS best practice in community pharmacies when antibiotics are requested,” says Dr Duerden, also a GRIP member and regular Pharmacy Magazine contributor.
“For example, keeping leaflets in the pharmacy that outline the self-limiting nature of most respiratory infections and the common durations of symptoms can be very helpful.”
“Many patients and healthcare professionals tend to underestimate symptom duration. For example, it is normal for a cough to persist for three weeks after a respiratory virus. Leaflets can also help as a safety net and advise when it is important to seek help, such as a sore throat in which swallowing is impaired.”
Dr Duerden also suggested using posters to advise about managing respiratory infections and the importance of reducing antibiotic use.
It is less than a century since Alexander Fleming made his momentous discovery. Today, resistance threatens to end the antibiotic era – but there are signs that AMS is beginning to make a difference.
Further resources
- FeverPAIN or Centor criteria
- GRIP has produced numerous resources for use by pharmacies, which are available in several languages. These include leaflets, posters and guides for talking to patients.
Sponsored
 Sponsored education
Sponsored education
Managing fever in children
Get to grips with the current guidance on managing fever in children and how antipyretics can help, and discover products you can recommend.
 Sponsored education
Sponsored education
7 steps to managing sore throat
Get to grips with what customers want from their sore throat treatment and upgrade your consultations with this 7-step guide


Record my learning outcomes